SPECIAL REPORT-Nipah virus outbreak renews calls to protect bat roosts
Share :
It was more than two weeks before doctors even realized what they were treating, the fourth outbreak in five years of the lethal, brain-swelling Nipah virus in India’s Kerala region.
It was more than two weeks before doctors even realized what they were treating, the fourth outbreak in five years of the lethal, brain-swelling Nipah virus in India’s Kerala region. By then, hundreds of people had been exposed to the bat pathogen. Halting the disease’s spread required deploying an army of workers, who put this village and eight others on partial lockdown for two weeks, surveyed more than 53,000 houses for signs of illness and tracked down 1,200 people who had come into contact with infected patients, according to the World Health Organization.
Ultimately, six people were infected, and two of them died. Though Kerala’s response to contain the outbreak drew international praise, the quick spread of the virus and its impact on tens of thousands of people illustrate what many scientists and world health leaders say is a weakness in public health policy: relying solely on disease containment. Governments, they say, must also control land development and protect animal habitats in areas where there is high risk of pathogens leaping from animals to people, a phenomenon known as spillover. The lesson comes at an important time, as global health leaders work on a legally binding accord for responding to future global health crises. Though many have been advocating for spillover prevention measures, a main difficulty in the negotiations so far has been balancing the needs of emerging economies against the risk of unchecked development. Because spillover risk is concentrated in lower income countries in the tropical south, the cost of preventing another pandemic falls squarely on nations that can least afford it.
Authorities in India’s national government say it’s a cost that can’t be ignored. Stopping bat viruses from spreading requires not just rapid response to outbreaks but careful monitoring of the bats themselves, said Subrat Mohapatra, a forestry official in India's environment ministry. To that end, federal and state officials say they are talking about ways to protect bat habitats in areas where spillover risk is high. “We have learned to manage the spillovers, but we have to constantly keep track of the high-risk zones as if they are volcanoes waiting to erupt,” Mohapatra said. Analysis of environmental conditions and other factors that contribute to spillover makes it possible to identify danger zones so that governments can take steps to reduce risk. An exclusive Reuters analysis in May provided a roadmap of such areas.
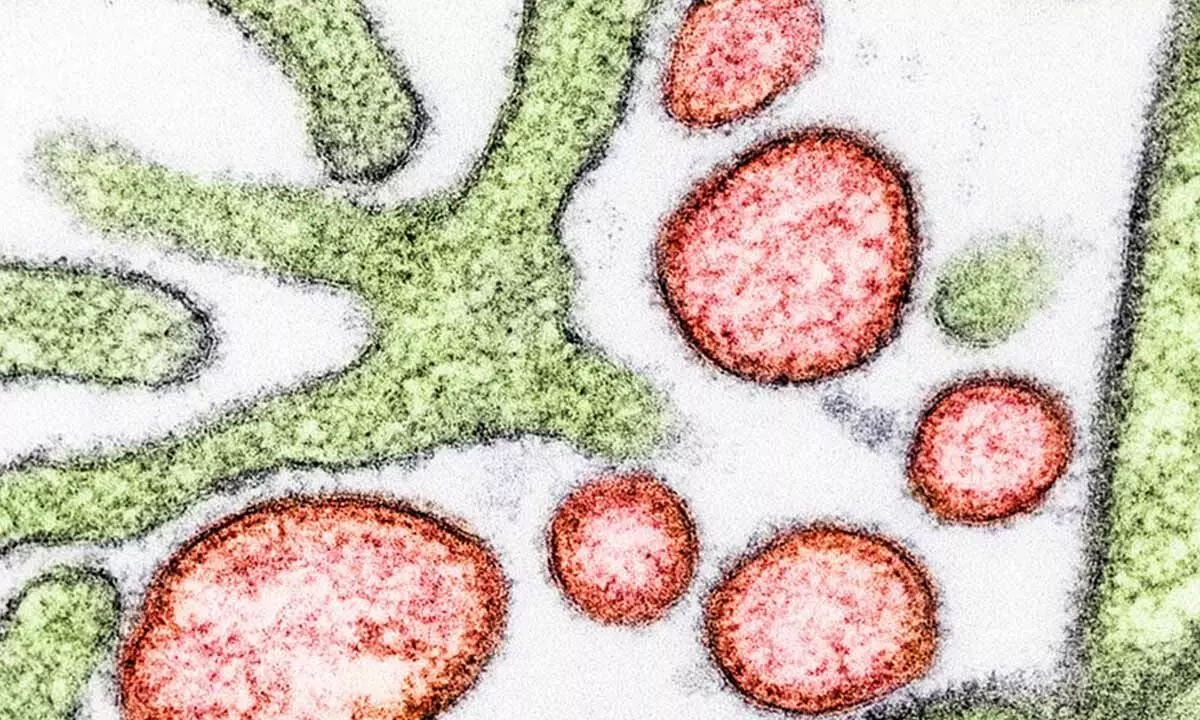
Reporters compared ecological conditions across the globe from 2002 through 2020 with those that existed at the time of past spillovers, identifying 9 million sq km – covering 6% of the Earth’s land mass – where conditions were ripe for pathogens to jump from bats to humans. Nearly 1.8 billion people lived in those jump zones in 2020, an increase of 57% since 2002. The analysis focused on bats because they are linked to many of the deadliest disease outbreaks of the past half century, including the recent COVID-19 pandemic. Though its specific source is still unknown, the virus that causes COVID-19 is related to coronaviruses found in some horseshoe bats, a type common in tropical Asia. Kerala is one of the likeliest places on earth for spillover to occur, the analysis showed.
SEEKING SOLUTIONS Bhupender Yadav, India’s minister of environment and forest, told Reuters that talks are underway between his agency and state officials over the need to create “ecological protection zones” in areas at high risk of Nipah spillover.
Kerala Health Minister Veena George said the state government has created a new Nipah research center in Kozhikode to investigate why spillover keeps occurring there and how to prevent it. Researchers will look at a wide range of factors, including tree loss, agricultural practices, urbanization and community awareness – and what government actions are needed to reduce risk. She cited protecting bat-roosting trees and planting native flowering trees – natural food for bats – as examples of what government could do. A federal initiative to identify and protect ecologically sensitive areas in the region, begun more than a decade ago, stalled after encountering protests from landowners and resistance from state and local governments eager to boost their economies.
That same conflict is challenging global health leaders today as they work on an accord to govern response to future global health crises. The World Health Organization’s 194 member states would be required under international law to adhere to the treaty. How they would be held accountable is among the issues still under debate. The latest draft, released by the WHO on Oct. 16, would require countries to conduct risk assessments for spillover as well as to “monitor and mitigate environmental factors associated with the risk of zoonotic disease spillover.” A growing body of research has linked deforestation, urbanization and intensive farming to spillover.
WHO delegates are expected to debate the proposal when they resume discussions on the treaty Nov. 6 in Geneva. Discussions thus far have focused on the need to better prepare for future outbreaks by addressing massive failures in the world response to the COVID-19 pandemic. Prevention proposals have lower income countries worried about costs and economic impact. “We are hearing that a number of governments in the Global South will not agree to this language unless wealthy countries agree to help finance these actions – a perfectly reasonable demand,” said Nigel Sizer, executive director of Preventing Pandemics at the Source, an international research and advocacy organization involved in the treaty talks.
In the U.S., the Biden administration has supported the treaty effort and contributed $450 million to the World Bank Pandemic Fund to help lower-income countries. But more funding is needed, Sizer said, and would require approval from a sharply divided Congress. The U.S. has pledged to transfer another $250 million this fiscal year, said former U.N. ambassador Pamela Hamamoto, the U.S. lead negotiator on the accord, in a written statement to Reuters. While congressional approval is needed, she said, "global health security has a legacy of strong bipartisan support."
The European Commission is "committed to the successful conclusion" of negotiations, a spokesperson said in an email to Reuters. The spokesperson did not reply to a question about whether the European Union would provide new funding. ‘BATS NEED INTENSE PROTECTION’
Nipah, which comes from bats and causes a lethal, brain-swelling fever in humans, has been linked to the deaths of two dozen people in Kerala since its first, surprise appearance here in 2018. A 1998-1999 epidemic in Malaysia killed at least 105. Hundreds more have died in near-annual outbreaks in Bangladesh since 2001. Nipah is classified as a priority pathogen by the WHO because of its potential to trigger an epidemic. There is no vaccine to prevent infection and no treatment to cure it. Investigators still don’t know precisely how the virus jumped from bats to people in each of the four Kerala outbreaks dating back to 2018. But bats roosting near homes and businesses have tested positive for Nipah, including in the latest outbreak. In three of the outbreaks, fruit or nuts with bite marks were found near where the initial patient fell ill. Scientists theorize those people got sick from eating or touching contaminated fruit or through direct contact with an infected bat’s saliva, urine, excrement or blood. In Bangladesh, research showed that people got Nipah after drinking date palm sap contaminated with bat saliva or urine.
Soon after the recent outbreak, a Reuters reporter saw giant fruit bats flying among cultivated trees on the land where the first victim, Muhammad Ali, grew coconut, banana and papaya. Ali’s wife said her husband knew about the risk of Nipah and was careful to avoid bat-bitten fruit. His symptoms began with a headache on Aug. 24 that progressed to high fever and delirium within days, she said. He was admitted to three hospitals before succumbing on Aug. 30. By then the virus had spread to their 9-year-old son and her brother. Both recovered. That recent outbreak and the three that preceded it followed increased tree loss near each victim’s home. Tree clearing spiked across Kerala after Pinarayi Vijayan, the state’s chief minister, took office in 2016 on a pro-development platform. After a slowdown during the COVID-19 pandemic, development is again on the rise as state leaders look to boost the economy.
In the Kozhikode district, where three of the four outbreaks happened, village governments have issued tens of thousands of building permits for new homes each year. The development carves away trees on the rolling hills that are prime habitat for the flying fox, a fruit bat that carries the Nipah virus. The extensive tree removal and development have created ideal conditions for spillover, according to a Reuters analysis of ecological data, much of it derived from satellites.
Even some of the bat roosts where investigators found Nipah after previous outbreaks have since been uprooted by development, Reuters found during a September visit. On the heels of so much development, bats are roosting in populated areas in extraordinary numbers, researchers say. They are attracted by fruit and nuts grown on farms and in home gardens, replacing the animals’ natural diet of flower nectar and wild fruit.
At least five colonies with hundreds of flying foxes have congregated in and around the village where the latest outbreak began, said Sreehari Raman, a Kerala Agricultural University bat scientist who assisted in the outbreak investigation. “I've never seen this kind of high density,” Raman said.
Research has found evidence that bats stressed by such disruptions can shed more virus, adding to the concerns, said Kerala Agricultural University Dean P.O. Nameer, who has been tracking the movement and breeding patterns of bats in the area. “We have devastated most of our habitats,” he said.
WHO WILL LEAD? The state government issued a “One Health” order in 2022 in response to recurrent outbreaks of Nipah, H1N1 and other zoonotic diseases. One Health, endorsed by the WHO and the United Nations, is a zoonotic disease control and prevention approach that links human health to animal health and protection of the natural environment. The order included calls for community surveillance to identify events that might trigger a disease outbreak -- such as dead birds that could signal the presence of bird flu -- and to prevent spread. But the order did not address the broader issues of deforestation, habitat loss or urbanization, which many scientists say are major drivers of spillover and an essential element of One Health. Bats are a leading source of zoonotic viruses, but a 2022 study found that less than half of Kerala’s bat habitat and only 10% of flying fox habitat are covered by state or federal government protections.
Many land use decisions fall on municipal governments, called panchayats. But the presidents of the villages where the first and most recent Nipah outbreaks happened told Reuters they did not have the wherewithal to consider spillover risk when governing the development of private land. The state would need to act to protect trees and bat roosts, they said. “Why that isn’t occurring still baffles me,” said Sajith Kizhakkayil, president of the village of Maruthonkara and a neighbor of the first victim who died. “When such a law is in place, it would be greatly beneficial.”
Vijayan, Kerala’s chief minister, did not respond to questions about the state’s role in spillover prevention. Unni Vengeri, president of Changaroth village, where the 2018 outbreak began, said that incident prompted village officials to ban the removal of flying fox roosting trees. But the restriction only applies to public property. Many trees have been cut on private land to make way for construction of large, new homes.
A 2022 study by Kerala scientists recommended preserving the large trees that provide food and shelter for bats in Kerala’s midland region and planting more native fruit trees to address the loss of bat habitat to development and quarry mining. Planting native trees also is getting attention from the international commission studying spillover. The commission, convened by the Lancet medical journal and the Coalition for Preventing Pandemics at the Source, a U.S.-based nonprofit organization, also will research ways to incentivize tree planting and to design public projects to minimize habitat loss.
The group also intends to study equitable solutions for spillover risk management, which falls most heavily on lower income countries in the tropical south, where Reuters analysis found the risk is highest. Those countries say they need more financial help from wealthier nations to cover the costs of prevention measures and the economic consequences of limiting deforestation and development. It is imperative that global treaty negotiators reach consensus on prevention, Dr. Francisco Pérez-Cañado of the European Commission said at an Oct. 16 World Health Summit panel in Berlin.
“Unless we will look at prevention linking animal health, environment and human health, we will not stop the next pandemic,” he said. “When the next pandemic comes, and we have millions and millions of citizens across the world dying, let it not be because we missed this one piece.”