Antibiotic Awareness Week (Nov. 18-24): Beware of bacterial predators
Antibiotics are effective only against bacterial and not viral infections. But a widely prevalent misconception that antibiotics are also effective in treatment of viral infections like cold and flu has resulted in over consumption of these drugs. Pathogenic bacteria can adapt to the presence of low dose antibiotics, and eventually form a population that is completely resistant to the antibiotic regardless of the dosage
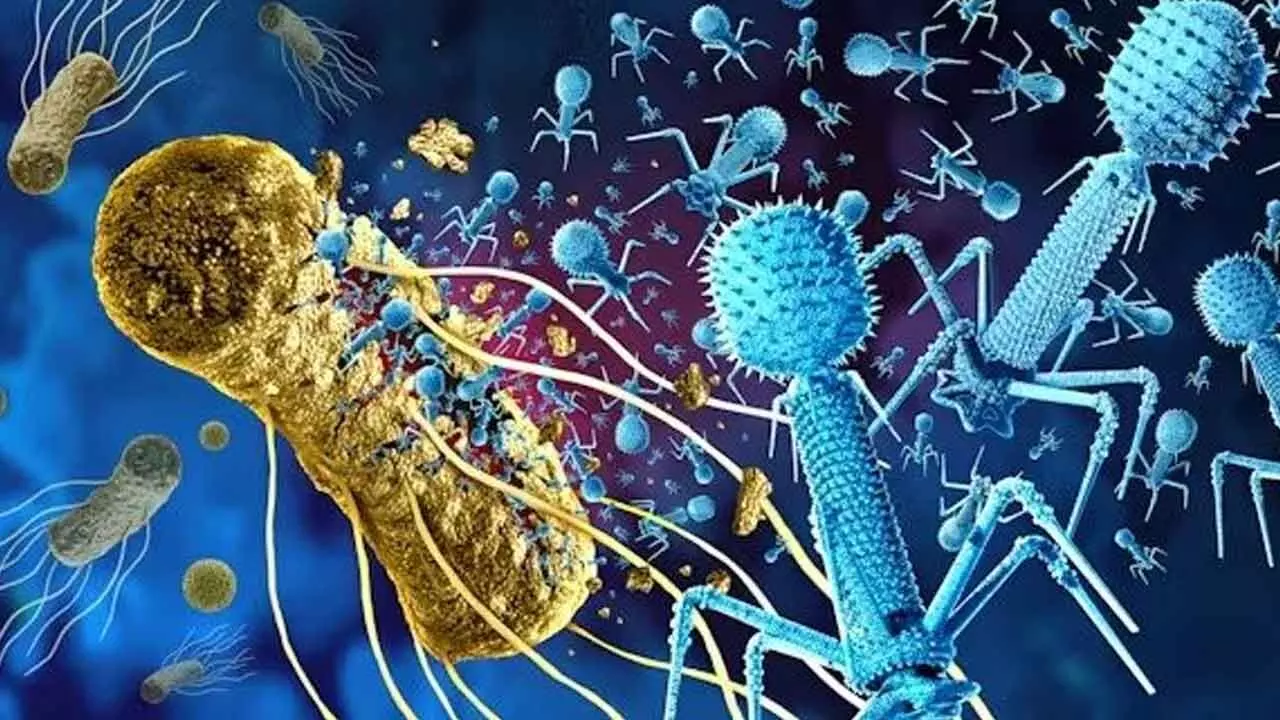
Indiscriminate consumption of antibiotics facilitated by their easy over-the-counter accessibility in India is spawning predators within our system which are as dangerous – if not more – as the prevalent viral perpetrators of dengue and other highly debilitating diseases. The common notion – supplemented by ignorance – that antibiotics are the panacea for all ailments, has become instrumental in creating reservoirs of drug resistant pathogenic bacteria. Bacterial resistance to antibiotics implies that the human body is fast losing its capability to fight infections and infectious diseases.
Since there is no alternative to antibiotics for the treatment of bacterial infections, the resistance to these drugs would mean the pathogens becoming unstoppable and the diseases caused by them untreatable. Such an eventuality is substantiated by a UK study, which warns that by 2050, antimicrobial-resistant infections could be the leading cause of death worldwide. The genesis of pathogenic bacteria developing resistance or immunity to drugs is attributed to overuse, underuse and misuse of antibiotics. Antibiotics are effective only against bacterial and not viral infections. But a widely prevalent misconception that antibiotics are also effective in treatment of viral infections like cold and flu has resulted in over consumption of these drugs.
India is one of the biggest antibiotic markets with the worst drug resistance index. The huge consumption in the country was fuelling antibiotic resistance among the Indian populace. According to Centre for Global Development (CGD), one of the main drivers of the problem of antimicrobial resistance (AMR) – an impending crisis which already causes over 1.25 million annual deaths globally and nearly 300,000 annual deaths in India – is the overuse of antibiotics. While access to antibiotics is key to prevent mortality, insufficient controls on prescription and dispensing can lead to high levels of unnecessary use and thus worrying increases in resistance. The report pointed out that striking the right balance between access and stewardship is a policy challenge for all countries
Self-medication without consulting doctors, and, on many occasions consuming the drugs on the advice of quacks, has triggered proliferation of resistant bacteria within the human system. According to medical experts, antibiotics needs to be strictly consumed according prescribed dosages and any deviation could lead to bacterial resistance. They point out that many of the patients either stop taking the tablets as soon they are cured of the ailment or continue to have more than the prescribed dosage. Such consumption patterns only make the pathogenic bacteria develop stronger defenses against the drugs.
Antibiotic dosages are designed to eradicate entire populations of the pathogens. When antibiotics are not taken for the entire prescribed course, pathogenic bacteria can adapt to the presence of low dose antibiotics, and eventually form a population that is completely resistant to the antibiotic regardless of the dosage. In an overpopulated scenario in the human system, while the susceptible pathogens are killed by the antibiotics, the survivors have the potential to develop immunity by absorbing small residual doses of the drug. Moreover, pathogenic bacteria also develop resistance or immunity due to mutation and by imbibing the immunity trait from the drug-resistant bacteria.
The World Health Organisation (WHO) has classified antibiotics into three categories – access, watch and reserve - on the basis of their safety standards and risk factors and recommended their usage accordingly. WHO recommends that Access group of antibiotics should be widely available and at an affordable cost and minimize the use of other two groups of antibiotics. Among the drugs in the Access group amoxicillin and Cloxacillin. Amoxicillin is used in the treatment of pneumonia, gonorrhea, meningitis, or infections of the stomach or intestines. Cloxacillin is used to treat a wide variety of bacterial infections. The Watch group includes antibiotics with high resistance potential when compared with the Access group and includes antibiotics such as third generation cephalosporin - antibiotics used to treat a wide variety of bacterial infections, such as respiratory tract infections, skin infections and urinary tract infections -fluoroquinolones - antibiotics that are commonly used to treat a variety of illnesses such as respiratory and urinary tract infections - and carbapenems- are a class of highly effective antibiotic agents commonly used for the treatment of severe or high-risk bacterial infections. The Reserve group includes antibiotics of last-resort like polymyxins, fourth and fifth generation cephalosporins.
Extensive Studies have revealed high resistance to broad-spectrum antibiotics like Fluoroquinolones and Cephalosporins in India both of which are most commonly prescribed for respiratory and urinary tract infections. Even the third-generation Ceftriaxone, has shown resistance. Erythromycin which is used in the treatment of fever, Ciprofloxacin - diarrhoea, Ofoxacin – cough, and, Amocxycillin - sore throat is reported to be among the overused antibiotics in India. The country has also developed the highest resistance rate against Flouroquinolones, Norfloxacin, Enoxacin, Ofoxacin, levofloxacin, Carbapenem; Meropenem, Imipenem and Colistin: Used for treating ventillator associated pneumonia and infections caused by other multidrug resistent bacteria. In addition to waning potency of drugs against general infections and infectious diseases, the proliferation of drug resistant pathogens assuming epidemic proportions is posing a more dangerous problem with the possibility of lethal complications in post-operative care.
Antibiotics are crucial in preventing infections during, and after surgeries including the recuperative stage to prevent infections and the presence of pathogens resistant to this line of treatment could prove to be fatal. Hospitals provide a conducive environment for the spread of the pathogenic, apart from other sources. With the medical world exhausting all lines of defence against the resistant pathogens and very few signs of alternatives in the pipeline till date, one of the solutions to prevent complications is to avoid self-medication and overconsumption, and follow the prescribed dosages recommended by the doctors.
(The writer is a senior print, electronic & digital media journalist)








