Testing the tests for SARS- CoV-2
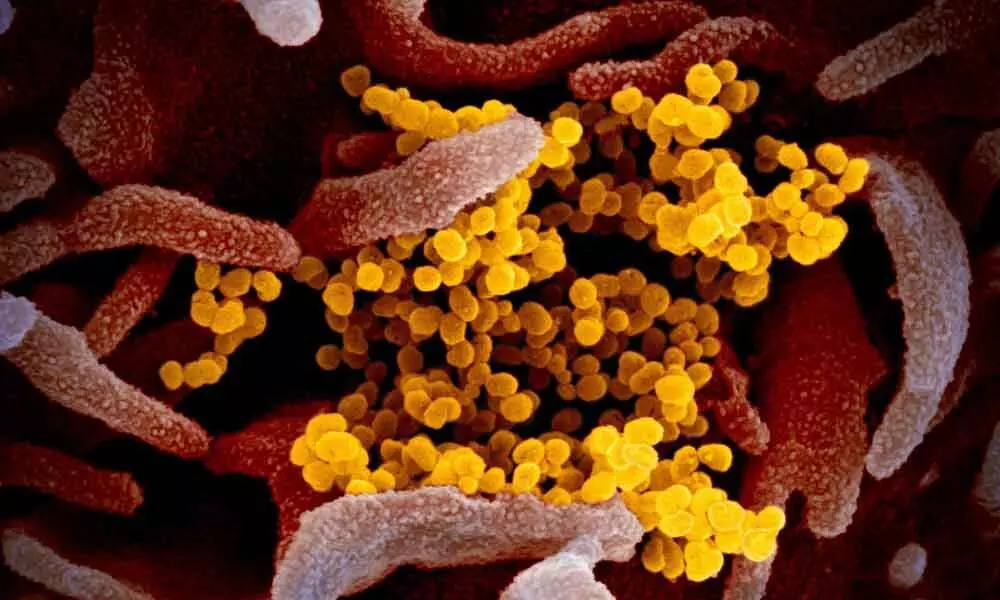
"Severe Acute Respiratory Syndrome Corona Virus 2 (SARS-CoV-2)" is the causative organism of "COVID-19," the disease which has metamorphosed into a veritable pandemic. The name itself is a code - 'CO' stands for 'corona,' 'VI' for 'virus' and 'D' for disease i.e. corona virus disease 2019. COVID-19 is now a household name and so are PCR and rapid antibody tests, the two major tests for COVID-19. Yet questions regarding the reliability of these tests haunt our minds. Can we be certain of having contracted the infection if we test positive? Can we heave a sigh of relief if we test negative? Let us search for these answers today.
Validity of a test
How to know that a test is accurate? The answer lies in its validity. Validity is the ability of a test to correctly separate those having disease from those who are disease-free. It has two components: sensitivity and specificity. Sensitivity is the ability of a test to correctly identify everyone having the disease whereas specificity is the ability of a test to correctly identify everyone who is disease-free (among those tested). We hardly find tests with one hundred per cent sensitivity as well as specificity. What becomes inevitable then? False negatives who test negative despite having the disease and false positives who test positive despite being disease-free. A highly sensitive test will have less false negatives. On the contrary, there will be less number of false positives in a highly specific test.
Dangers of false negatives and positives
False-negative tests give a false sense of security. Such patients get delayed or no treatment whereas they continue to spread infection. As governments across the world plan to relax restrictions and loosen lockdowns in a bid to reopen economies, there is a serious risk that people who are wrongly believed to be disease-free because of their false negative test results will cause a re-infection in society. Hence, we must select tests with high sensitivity so that false-negative results are minimized. On the contrary, every false-positive result causes a healthy person to unnecessarily undergo isolation as well as retesting. People getting false positive results in antibody tests may be misguided to believe that they are immune to COVID-19 as they have the protective antibody and they may negligently get exposed and infected. Therefore, false positive results also need to be avoided.
RT-PCR test: false positives & false negatives
All validated RT-PCR tests have high specificity because they detect specific gene sequences of the RNA of SARS-CoV-2. Hence, false positive results are rare here. But beware! RT-PCR test can sometimes produce false-negative results. An infected patient may even test negative several times before testing positive. Therefore, correlation with history of travel and contacts, clinical observations, chest X-rays and chest CT scans is recommended in suspected COVID-19 patients who test negative. Retesting is also advised in such cases, 2 to 4 days after the first test.
RT-PCR test: causes of false-negative results
RNA samples for RT-PCR test are usually collected from swabs of naso-pharynx or oro-pharynx e.g. throat. However, RNA samples are relatively unstable because enzymes that can split RNA are found in many places including the surface of the human body. Therefore, if the samples are transported to the laboratory within 72 hours after collection, the swabs are placed in tubes containing viral transport medium (VTM) and stored at 2 to 8°C (cold chain). If testing is delayed further, specimens must be stored at -70°C or below or transported on dry ice. Meticulous maintenance of these conditions for storage and transportation of samples will prevent RNA-splitting enzymes from degrading viral RNA in those samples. Failure to ensure the prescribed environmental conditions may obviously cause false-negative results.
Besides, swab must be taken from a spot sufficiently back inside the throat to get a viable sample for this test. Otherwise sample quality may be poor, leading to false-negative result. False negative results also occur due to improper reagents, poor technique in conducting the test in the laboratory because of lack of trained laboratory personnel and in very early or late stages of the disease when low levels of the virus are present. Besides, failure to amplify the target sequences of viral RNA during processing of the sample in the laboratory may cause false-negative results. False-negative results may also happen during the later stage of infection as virus may no longer be present in the upper respiratory tract i.e. naso-pharynx or oro-pharynx at that time. To avoid false negative reports, specimens can then be collected from the lower respiratory tract i.e. trachea/windpipe and below where the virus will still be present.
Rapid antibody test:
dilemma faced by governments/regulators
Amidst the frenzy of launching antibody tests on a huge scale at the earliest, we must not forget the crucial issue of reliability of those testing kits. In view of the current public health emergency, the Food & Drug Administration (FDA) in USA have issued emergency use authorization (EUA) to private companies for using their medical devices and kits despite the lack of adequate data to prove their accuracy. Many other countries have relaxed criteria for validating antibody testing kits or imported them in a hurry, only to find later that the results they yield are highly inaccurate. It is the need of the hour for the government and national regulators to do a proper balancing act so that the need for accuracy of any new diagnostic test is not sacrificed at the altar of public health urgency.
Rapid antibody tests: false
positives & false negatives
These tests usually detect antibodies that are produced in the human body against the spike protein of SARS-CoV-2. Why is this protein selected? Because this is the main antigen that attaches to the host cell, facilitates entry of the virus into the host cell and elicits neutralizing antibodies. Unfortunately, some antibody test kits also detect antibodies produced in the human body against the spike protein of other corona viruses because the antigenic structures of the spike proteins of SARS-CoV-2 and common cold-causing corona viruses have probably about 50 to 60% identity. Such kits will obviously yield some inaccurate results as someone infected with some other corona virus may falsely test positive. To eliminate the potential for such cross-reactivity, new antibody tests must select sections of the spike protein of SARS-CoV-2 that are completely dissimilar from all other corona viruses. Another problem arises when some antibody test kits are validated with samples from patients who are severely diseased and will develop a strong antibody response. Such antibody test kits may be reasonably accurate in severely ill patients but they may give false-negative results in patients with mild or no symptoms who usually have less viral load and produce fewer antibodies in their blood.
We must also note that antibody response may be low with advanced age, poor nutritional status, less severity of disease (low viral load) and in the presence of immunodeficiency disorders (e.g. AIDS) or with regular intake of immunosuppressive drugs (e.g. steroids in high dose). Antibody test may be negative in all such cases even if someone has recent or past infection.
Way forward
No country in the world has yet tested all its inhabitants for COVID-19 because every nation aims to ensure optimal utilization of its available resources. Nevertheless, it is being widely acknowledged today that massive ramping up of testing for COVID-19 is crucial to permanently control this public health crisis, irrespective of the date we decide to relax lockdown measures in our country. Meanwhile, there is a pressing need to ensure that all the tests done are accurate and their outcomes are rightly interpreted so that doctors as well as policymakers are not misguided while taking decisions. In order to cater to the burgeoning needs for testing in the foreseeable future, every nation must massively invest in the technology and infrastructure of the medical diagnostics industry, continuously improve the quality of indigenously manufactured kits, research and invent newer testing methods that yield more accurate results in less time and ensure the availability of sufficient number of trained manpower for proper sample collection and testing. As aptly said in Purusha Sukta of Rig Veda, "Nanya pantha vidyate ayanaya" i.e. there is no other way on earth.
(The author is Inspector General of Police in Andhra Pradesh and alumnus of ISB, Hyderabad. The views expressed are his own and not those of the Government)









